The human brain is one of the most complex structures in existence. It controls every thought, movement, and emotion we experience. When something goes wrong within it, the effects can be life-changing. Diagnosing brain conditions is one of the most intricate tasks in medicine, requiring both advanced technology and deep expertise. Neurosurgeons—specialists trained to treat disorders of the brain, spine, and nervous system—play a critical role in identifying these conditions accurately before planning treatment.
This article explores how neurosurgeons diagnose brain conditions step by step, from the first consultation to the use of sophisticated imaging and diagnostic tests.
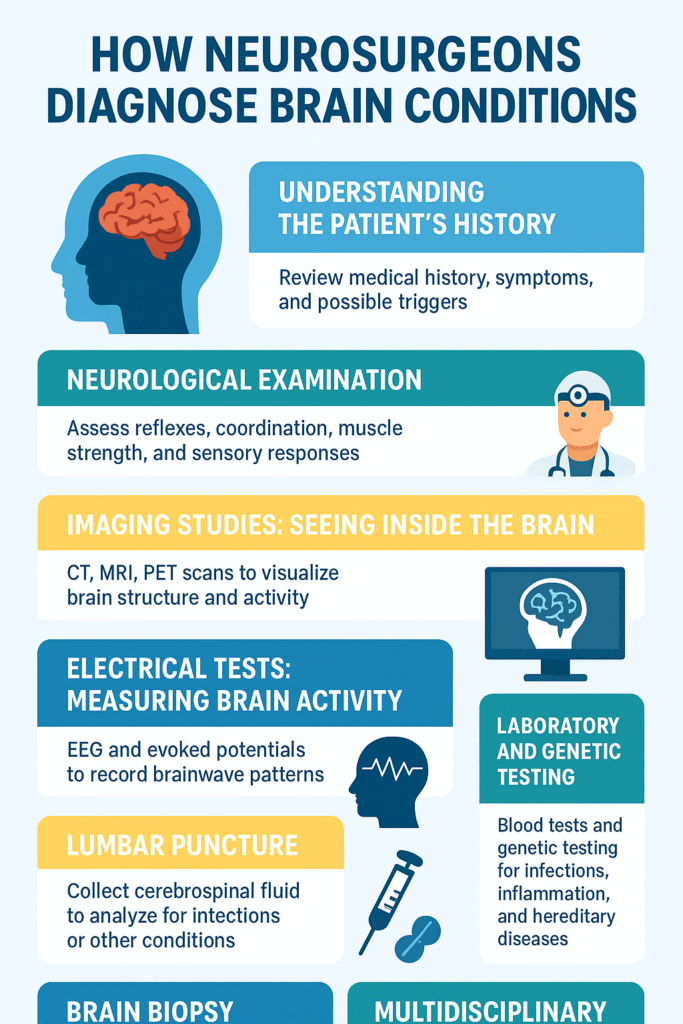
1. Understanding the Patient’s History
Every diagnosis begins with a story. When a patient visits a neurosurgeon, the first step is a detailed review of medical history. This includes understanding symptoms, their duration, and possible triggers.
The neurosurgeon asks questions like:
- When did the symptoms start?
- Are they constant or do they come and go?
- Have you had any recent injuries or infections?
- Is there a family history of neurological disorders?
This step helps narrow down possible causes. For instance, a history of trauma may point toward a brain injury, while a family pattern might raise suspicion of hereditary disorders like Huntington’s disease.
Sometimes, symptoms such as persistent headaches, seizures, or balance issues can be linked to several different conditions. That’s why a thorough history is vital—it sets the stage for targeted testing.
2. Neurological Examination
After taking the patient’s history, the neurosurgeon performs a neurological exam. This physical assessment helps evaluate how the brain and nervous system are functioning.
The test focuses on key areas such as:
- Reflexes: Checking how quickly nerves respond to stimuli.
- Coordination and balance: Assessing walking, standing, and finger-to-nose movement.
- Muscle strength and tone: Looking for weakness, stiffness, or involuntary movements.
- Sensory responses: Testing the ability to feel touch, temperature, and pain.
- Cranial nerves: Evaluating vision, hearing, facial movement, and speech.
Each test provides clues about which part of the brain or nervous system might be affected. For example, slurred speech or facial drooping could indicate a problem in the brain’s left hemisphere, where language control is located.
3. Imaging Studies: Seeing Inside the Brain
Once the neurosurgeon has a clinical impression, the next step is imaging. Modern technology allows doctors to visualize the brain’s structure and activity with incredible detail.
CT Scan (Computed Tomography)
A CT scan uses X-rays to produce cross-sectional images of the brain. It’s often the first imaging test done, especially in emergencies like head injuries or strokes. A CT can quickly detect bleeding, skull fractures, and major tumors.
MRI (Magnetic Resonance Imaging)
An MRI provides a much more detailed view than a CT scan. It uses powerful magnets and radio waves to create 3D images of the brain. Neurosurgeons rely on MRI scans to detect tumors, brain infections, demyelinating diseases like multiple sclerosis, and even small structural abnormalities.
There are different MRI techniques, such as:
- Functional MRI (fMRI): Shows brain activity during tasks like speaking or moving.
- Diffusion Tensor Imaging (DTI): Maps white matter tracts to evaluate brain connectivity, useful in surgical planning.
- MR Angiography (MRA): Focuses on blood vessels to detect aneurysms or blockages.
PET Scan (Positron Emission Tomography)
PET scans measure brain metabolism using radioactive tracers. They help identify areas of the brain that are overactive or underactive, which is particularly useful in epilepsy and Alzheimer’s diagnosis.
4. Electrical Tests: Measuring Brain Activity
Sometimes, imaging alone can’t explain the cause of symptoms. In such cases, neurosurgeons turn to tests that record the brain’s electrical activity.
EEG (Electroencephalogram)
An EEG records brain wave patterns through electrodes placed on the scalp. It’s often used for diagnosing seizure disorders, sleep disorders, or encephalopathies. By analyzing wave patterns, doctors can pinpoint abnormal electrical discharges in specific brain regions.
Evoked Potentials
These tests measure the brain’s response to specific stimuli, like light flashes or sounds. They are helpful in detecting nerve pathway problems caused by conditions such as multiple sclerosis.
5. Laboratory and Genetic Testing
Some brain disorders have biochemical or genetic origins. Blood tests can reveal infections, inflammation, or autoimmune activity that affects the brain. For instance:
- Elevated white blood cell count may indicate meningitis or encephalitis.
- Abnormal hormone levels could signal pituitary gland issues.
In certain cases, neurosurgeons recommend genetic testing. This is particularly relevant for inherited conditions like neurofibromatosis, tuberous sclerosis, or certain types of epilepsy. Identifying the genetic cause helps in understanding disease progression and planning long-term care.
6. Lumbar Puncture (Spinal Tap)
When infections, bleeding, or autoimmune diseases are suspected, neurosurgeons may order a lumbar puncture. In this procedure, a small amount of cerebrospinal fluid (CSF) is collected from the lower spine using a needle.
The CSF is then analyzed for signs of infection, inflammation, or cancer cells. For example, high protein levels may indicate multiple sclerosis, while the presence of bacteria points to meningitis.
Although this test might sound intimidating, it’s a routine procedure performed under sterile conditions and local anesthesia.
7. Brain Biopsy
In rare and complex cases, when imaging and other tests are inconclusive, a brain biopsy may be needed. This involves removing a tiny sample of brain tissue for examination under a microscope.
It’s mainly used to confirm or rule out conditions like brain tumors, infections, or inflammatory diseases. The biopsy helps identify the exact type of tumor or lesion, which is critical for choosing the right treatment—surgery, radiation, or medication.
8. Multidisciplinary Consultation
Neurosurgeons rarely work alone when diagnosing brain conditions. They collaborate with neurologists, radiologists, oncologists, and pathologists. This multidisciplinary approach ensures that every detail is reviewed from different medical perspectives.
For example, a radiologist interprets scans, a pathologist studies tissue samples, and a neurologist provides insights into symptoms and medication management. Together, this team effort leads to an accurate and complete diagnosis.
9. Monitoring and Follow-Up
Diagnosis doesn’t end after one test. Many brain conditions require ongoing monitoring. Neurosurgeons may schedule repeat MRIs or CT scans to track tumor growth, swelling, or post-surgical healing.
In conditions like epilepsy or Parkinson’s disease, regular check-ups help assess how well treatments are working and whether adjustments are needed.
10. The Human Side of Diagnosis
While technology plays a huge role, the art of diagnosis still depends on the neurosurgeon’s judgment, experience, and empathy. Understanding a patient’s fears, explaining results clearly, and discussing treatment options honestly are all part of the diagnostic process.
For patients, the journey can be emotionally taxing. But knowing that each test, scan, and consultation brings them closer to answers often provides comfort and hope.
Conclusion
Diagnosing brain conditions is both science and skill. It begins with careful listening and observation, followed by cutting-edge imaging and precise testing. Neurosurgeons combine their deep knowledge of the brain with advanced diagnostic tools to uncover the exact cause of symptoms.
From CT and MRI scans to EEGs and biopsies, every step is designed to reveal what’s hidden within the brain’s intricate network. Accurate diagnosis is the first and most crucial step toward effective treatment—and ultimately, toward helping patients regain control over their health and lives.

Doctor Manish Rawat, the best neurosurgeon in Gurugram, is a highly accomplished Senior Neurosurgeon with over 25 years of medical experience, including 18 years dedicated to neurosurgery.

